What is a Mallet Finger?
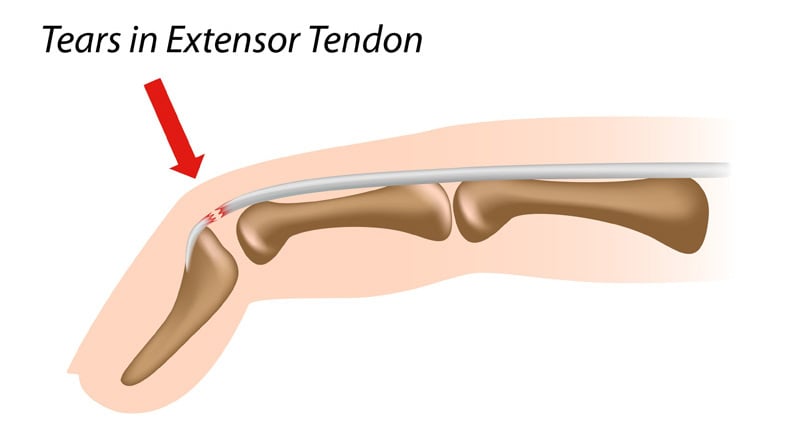
Mallet finger injuries usually occur due to a sudden jamming of the fingertip which results in either fracture (mallet fracture) or tendon rupture at the base of the fingernail. The result is a “drooping” deformity of the end of the finger with inability to straighten the end of the finger. These are very common and often occur after relatively mild injuries.

Causes
Most causes of mallet fingers involve trauma to the fingers:
- Sudden “jamming” injuries to the fingers (sometimes very mild injuries)
- Blunt force trauma (work injuries, sports, vehicle accidents)
Signs and symptoms
Symptoms of a mallet finger usually include one or more of the following:
- Finger pain and tenderness to touch (usually mild at the base of the fingernail)
- Finger swelling / stiffness
- Finger bruising
- Finger deformity (end of finger droops and won’t straighten)
Is there a test for mallet finger?
Mallet finger due to tendon rupture can usually be diagnosed by physical exam. We usually obtain an X-ray to see if there is an associated fracture (mallet fracture).
Treatment
Most mallet finger and even mallet fractures can be treated nonoperatively, but occasionally surgery is required. It is important to start treating these as soon as possible, and to stick to the treatment recommendations very carefully as delayed care and noncompliance with splinting often result in poor outcomes, including permanent drooping of the finger, nonunion (nonhealing of the fracture), and sometimes painful arthritis of the finger joint.
Nonoperative treatment:
Splinting is the mainstay of treatment for most mallet fingers and mallet fractures. A small splint is applied to the end joint of the finger, allowing the other two joints to move. The end joint of the finger must be held straight at all times, as allowing it to bend even for a moment can reset the clock for healing or prevent healing altogether. We will show you techniques for cleaning and inspecting the skin of the finger under the splint without allowing the end joint to bend, then replacing the splint. We typically recommend six weeks of full-time splinting (removing only for hand hygiene), followed by 6 weeks of wearing the splint during high-risk manual activities and also at night-time. Occasionally, more than one round of nonoperative treatment is attempted if the deformity recurs.


stax splint and alumafoam splint for mallet finger
Operative treatment:
We recommend surgery to repair larger mallet fractures that allow the end joint of the finger to slip out of alignment. X-rays are useful to determine which mallet fractures need surgery. We administer mild sedation, numb the finger, and place two or three metal wires through the skin and into the bone to hold the fracture pieces and joint in the proper alignment while it heals.
Ready to confirm a diagnosis and fix the problem, or just want to learn more?
Our board-certified orthopedic hand and wrist surgeons, Eric Angermeier, MD and Kyle Kokko, MD, PhD, are here to help! They can often diagnose the problem in one visit, and get you started with a treatment plan. We offer a wide variety of both nonoperative and operative treatment options.
Call today for a clinic or telehealth appointment! 854-429-4263